Early Total Cervix Occlusion (ETCO)Erich Saling MD FRCOG and Monika Schreiber MD(Translation into English: Amos Grunebaum MD FACOG, Cornell University, New York) This information is geared towards patients who previously had one or more late miscarriage or preterm birth and for whom the Early Total Cervix Occlusion is being considered. |
||||||||||||||||||||||||||
|
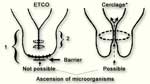
What is an Early Total Cervix Occlusion (ETCO)?Contrary to the less successful cerclage where the cervix is only tightened, with the total occlusion the cervix is operatively completely closed using sutures and subsequent healing (see image 1). The ETCO closes the cervix completely and therefore prevents the ascension of bacteria from the vagina into the uterus by introducing a barrier. With the “early” TCO the cervix is closed between 12 to 16 completed weeks of the pregnancy and before anatomic changes in the cervix are found.
Caution!
|
|||||||||||||||||||||||||
|
|
Who should have an early cervix occlusion?There are many different etiologies for miscarriages and preterm births. Miscarriages in the early part of the pregnancy, before 12 gestational weeks, often have different causes than miscarriages later on in pregnancy and preterm births. Between 12 and 32 weeks, ascending genital infections are usually the main reason for such late miscarriages and preterm births and they often cause early labor and premature rupture of the membranes. Ascending genital infections are fortunately rare. The majority of pregnant women have a biologically undisturbed vaginal flora which is a good condition for prevention of infections. In some women there is an imbalance in the vaginal flora, and in those cases it’s usually sufficient to identify it early on and treat it. However, early detection and treatment does not appear to be sufficient in those women with recurrent late miscarriages or very preterm births. In those cases we suggest the Early Total Cervical Occlusion as a preventive measure. The ETCO is indicated in women who have a history of two or more miscarriages or preterm births between 12 and 32 weeks of the pregnancy and which was caused by an infection or there was no other cause found. After the first adverse outcome between 12 and the 32 weeks, one can consider the “small” ETCO instead of the “extensive” one. (The difference between the two is illustrated in the left part of image #1.) Besides, there is some experience which entitles to perform an ETCO generally in multiple pregnancies. From our perspective, it should be definitely considered when there are additional risk factors (e. g. after in-vitro fertilisation, or when a pregnant woman is near the end of her possible reproductive time). |
|||||||||||||||||||||||||
|
|
When should the Early Total Cervical Occlusion be performed?Prior to 12 completed gestational weeks there are usually other causes of a miscarriage such as genetic issues. Therefore the ETCO should be performed if possible at 12 completed and not later than at 16 completed weeks of the pregnancy and before there are anatomic changes in the cervix. After 16 weeks success rates decrease. |
|||||||||||||||||||||||||
|
|
How is the occlusion done?Prior to the procedure it’s necessary to exclude an infection. In addition, the vagina is carefully disinfected and in some hospitals an antibiotic is given. The procedure can be performed under general, spinal or epidural anesthesia. The surface is first removed to improve healing and the cervix is then closed and stiched in several layers. The left part of illustration 1 shows the result. Depending on individual risks and findings, it is suggested that the patient stays in hospital for several days. |
|||||||||||||||||||||||||
|
|
What happens before and during the labor?When labor starts, but no later than 37 weeks of gestation the scar tissue is opened with a small incision. This procedure can be done under local anesthesia and if there are no complications the pregnant woman can go home afterwards. A vaginal delivery is not only expected but suggested because the cervical dilatation during birth can be advantageous for later reconstitution of the cervix. |
|||||||||||||||||||||||||
|
|
Can a woman get pregnant again after a cervical occlusion?There are some women who had several successful pregnancies with repeated cervical occlusion. |
|||||||||||||||||||||||||
|
|
How successful are pregnancies after a cervical occlusion?The ETCO cannot prevent all miscarriages and
preterm births. Besides an ascending infection there are several
other causes of miscarriages and preterm birth such as abruptio
placentae, and preeclampsia which often require an early
pregnancy termination. In addition, other infections such as
untreated urinary tract infections can lead to preterm
birth. Nevertheless, our success rates with the ETCO are excellent. A recent publication reports that with the ETCO in 315 pregnancies in the period 2008–2011 a success rate of 95 % could be achieved, and with the so-called secondary cervical occlusion (late TCO) still a success rate of around 90 %. |
|||||||||||||||||||||||||
|
|
Are there increased risks because of the ETCO?Generally with this procedure, there are only slight risks to mother or child. When compared to a “normal” pregnancy or delivery there may be an increased risk of cervical scar developing after the surgery, but cases of cervical injury are rare. Naturally, there are the usual risks of any surgery such as risks from the anesthesia. That’s why the ETCO should only be performed when there are concrete indications. In follow-up studies of children born after a cervical occlusion over 90 % of them were normally developed. This number is similar to the average population development. |
|||||||||||||||||||||||||
|
|
Where is the cervix occlusion done?The cervix occlusion procedure is a special surgical operation which is done only in certain hospitals. The advantage of having someone to perform the procedure who has sufficient experience and has done enough of them justifies several hours of travel. We have particularly for Europe some contact information if your doctor does not know where your nearest hospital is, which offers this service. |
|||||||||||||||||||||||||
|
|
What else should be considered?We suggest not to have sexual intercourse until
the surgical scar has healed (mostly within 3–4 weeks). During
the follow-up visits your doctor can determine how far the
healing process has progressed and whether the wound has healed.
In addition, we suggest you attend your usual prenatal care
visits. Especially in couples with a history of miscarriages or preterm deliveries the next pregnancy is often associated with a lot of fear and concern. For many couples it may therefore be a good idea to get psychological support and exchange experiences with other involved couples (addresses for self-help groups can be found via internet). |
|||||||||||||||||||||||||